What Is Mesenchymal Stem Cell Lineage?
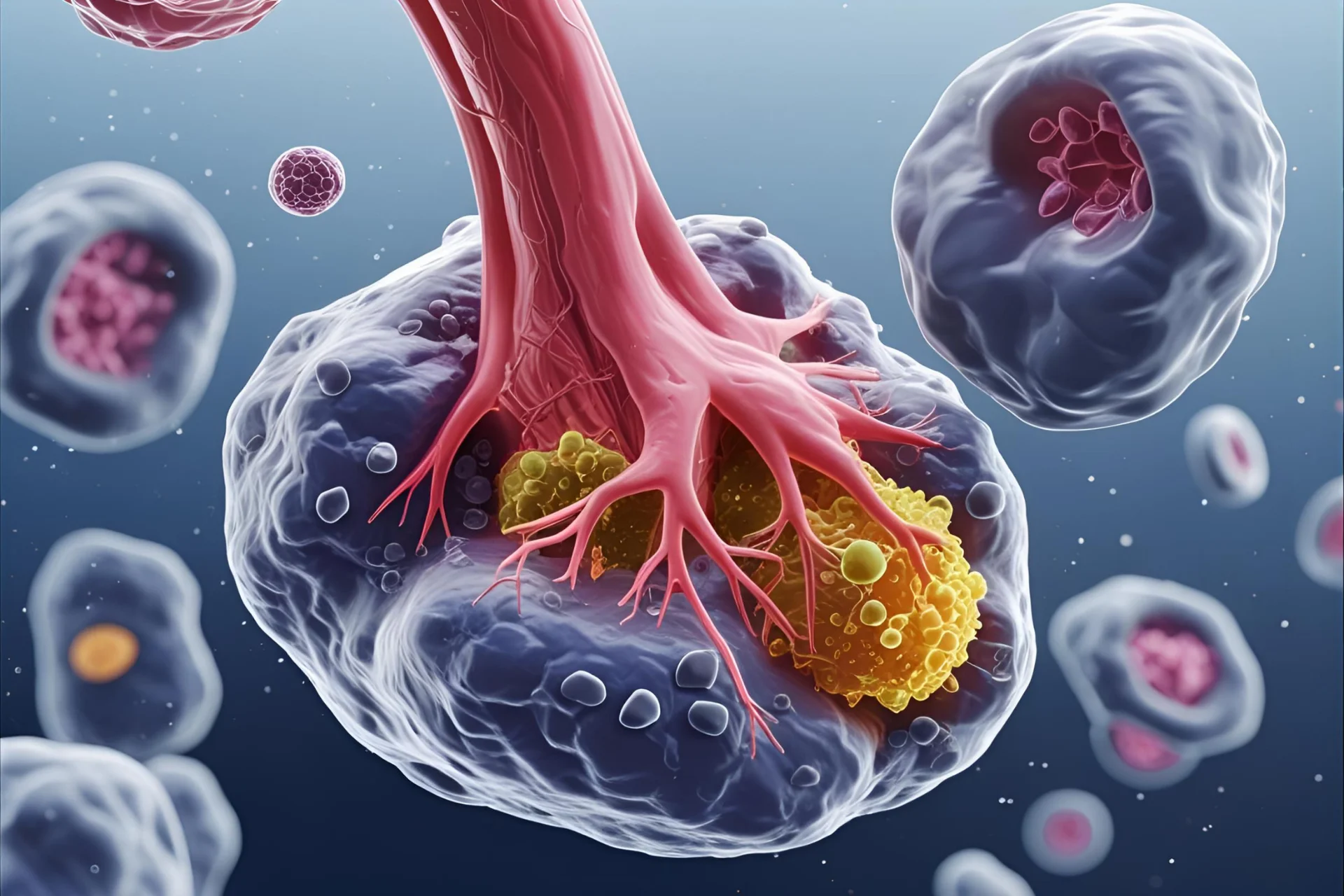
Mesenchymal Stem Cells (MSCs) are multipotent adult stem cells capable of self-renewal and differentiation into various mesodermal cell types. They are non-hematopoietic and typically adhere to plastic in standard culture conditions.
MSCs are derived from the mesoderm, the middle germ layer in embryonic development. This origin enables them to give rise to connective tissue cells, including bone (osteoblasts), cartilage (chondrocytes), and fat (adipocytes).
MSCs are multipotent, meaning they can differentiate into several but not all cell types. Their ability to regenerate damaged tissues, modulate immune responses, and promote healing makes them a cornerstone in regenerative medicine and cell-based therapies.
Understanding MSC Lineage Differentiation
In stem cell biology, “lineage” refers to the specific path a stem cell follows as it matures into a specialized cell type. For mesenchymal stem cells (MSCs), this typically includes osteogenic (bone), chondrogenic (cartilage), and adipogenic (fat) lineages, all originating from the mesodermal germ layer.
Lineage commitment is the point at which an MSC becomes dedicated to a specific differentiation path, influenced by internal and external signals. However, MSCs retain a degree of plasticity, meaning their fate can still be modified under certain conditions, such as exposure to different growth factors or environmental cues.
The stem cell niche, or microenvironment, plays a crucial role in directing MSC behavior. Growth factors like TGF-β, BMPs, and Wnt proteins regulate lineage-specific gene expression, while factors such as oxygen levels, matrix stiffness, and mechanical stress can push MSCs toward different lineages. Understanding and controlling these signals is key for targeted regenerative therapies.
Trilineage Differentiation Potential of MSCs
One of the defining features of mesenchymal stem cells (MSCs) is their ability to differentiate into three primary cell types: osteoblasts, chondrocytes, and adipocytes.
This is known as trilineage differentiation potential and is a critical criterion for identifying true MSCs, as defined by the International Society for Cell & Gene Therapy (ISCT).
These three lineages correspond to bone, cartilage, and fat tissue, making MSCs highly valuable in both regenerative research and clinical applications.
Osteogenic Lineage
MSCs can differentiate into osteoblasts, the cells responsible for forming new bone. This process is essential in bone regeneration, fracture healing, and orthopedic tissue engineering.
Markers:
MSCs are widely used in preclinical and clinical studies for treating osteoporosis, bone defects, and spinal fusion procedures.
Chondrogenic Lineage
Under the right conditions, MSCs differentiate into chondrocytes, the primary cells in cartilage. This pathway is of particular interest in cartilage repair for conditions such as osteoarthritis and traumatic joint injuries.
Markers:
Chondrogenic MSC therapies are being tested using scaffold-based delivery systems and hydrogel matrices to enhance integration and longevity of cartilage tissue.
Adipogenic Lineage
MSCs also differentiate into adipocytes, or fat cells, which are important in studying metabolic diseases and fat tissue engineering.
Markers:
Though less targeted for therapy, adipogenic MSC differentiation plays a vital role in understanding obesity, insulin resistance, and tissue regeneration involving soft fat-based structures.
Additional Lineage Potentials (Under Investigation)
Beyond the well-established trilineage pathways, mesenchymal stem cells (MSCs) are also being studied for their potential to differentiate into other specialized cell types. These include myogenic (muscle), neurogenic (nerve), and cardiomyogenic (heart) lineages. While these extended differentiation capacities are still under investigation, early results have opened new avenues in regenerative medicine and disease modeling.
Myogenic Potential (Muscle Cells)
MSCs have shown the ability to differentiate into myoblast-like cells under specific conditions involving growth factors like bFGF and mechanical stimulation. This has implications for skeletal muscle repair in muscular dystrophy and injury recovery.
Methods for Lineage Confirmation
Verifying the differentiation potential of mesenchymal stem cells (MSCs) requires a multi-step approach. Researchers commonly use in vitro culture techniques, lineage-specific staining, and molecular assays to confirm that MSCs have committed to a specific cell lineage.
In Vitro Differentiation Protocols
MSCs are first exposed to lineage-specific induction media to direct them toward osteogenic, chondrogenic, or adipogenic pathways. These media contain carefully selected supplements—such as dexamethasone, β-glycerophosphate, and ascorbic acid for osteogenesis; TGF-β3 and insulin for chondrogenesis; and IBMX and indomethacin for adipogenesis. These protocols typically span 14 to 21 days, allowing sufficient time for cells to initiate and maintain lineage-specific development.
Lineage-Specific Staining (Alizarin Red, Alcian Blue, Oil Red O)
After differentiation, histological stains are applied to visually confirm lineage commitment. Alizarin Red S binds to calcium deposits, indicating osteogenic activity. Alcian Blue stains glycosaminoglycans in the cartilage matrix, confirming chondrogenic differentiation. Oil Red O highlights lipid droplets in adipocytes, used as a marker for adipogenic lineage. These staining methods are quick and visually effective but typically require further molecular validation.
Gene Expression and Immunocytochemistry
To confirm lineage identity at the molecular level, researchers analyze gene expression and perform immunocytochemistry (ICC). RT-qPCR is used to measure lineage-specific gene expression—such as Runx2 for osteogenesis, Sox9 for chondrogenesis, and PPARγ for adipogenesis. ICC uses fluorescent or chromogenic antibodies to detect proteins like ALP, Aggrecan, and FABP4, allowing precise visualization of cell identity and confirming that the MSCs have successfully differentiated.
Factors Influencing Lineage Commitment
The lineage commitment of mesenchymal stem cells (MSCs) is not a passive process—it is actively shaped by a range of intracellular signals and external environmental cues. Understanding these influencing factors is essential for controlling MSC differentiation in both research and therapeutic applications.
Gene Expression and Immunocytochemistry
Key molecular signaling pathways play a central role in directing MSC fate. The Wnt/β-catenin pathway promotes osteogenesis and suppresses adipogenesis. TGF-β signaling is essential for chondrogenic differentiation and also regulates the balance between proliferation and differentiation. Bone Morphogenetic Proteins (BMPs), especially BMP-2 and BMP-7, strongly induce osteogenic lineage commitment. These pathways interact with each other and can be modulated to guide MSCs toward a desired lineage.
Mechanical Cues and ECM Interaction
Mechanical stimuli and interaction with the extracellular matrix (ECM) also affect lineage outcomes. Substrate stiffness, for example, influences differentiation: stiffer matrices promote osteogenesis, while softer environments may favor adipogenesis. MSCs sense mechanical tension and surface topography through integrins and mechanosensitive ion channels, which in turn activate intracellular signaling cascades that impact gene expression and cell behavior.
Hypoxia and Epigenetic Regulation
Environmental factors like oxygen tension (hypoxia) significantly influence MSC differentiation. Mild hypoxia tends to enhance chondrogenic and stemness-related gene expression while suppressing unwanted lineage drift. At the same time, epigenetic regulation, including DNA methylation, histone modification, and non-coding RNAs, plays a key role in stabilizing lineage-specific gene programs. These reversible modifications can be manipulated to either maintain MSC multipotency or promote irreversible lineage commitment.
Together, these biological and environmental inputs form a highly dynamic network that governs MSC lineage decisions. By carefully modulating these factors, researchers can enhance the precision and efficacy of MSC-based therapies.
Clinical Relevance of MSC Lineage Understanding
Understanding mesenchymal stem cell (MSC) lineage commitment is crucial for the success of regenerative medicine. Properly directed MSCs enable targeted tissue repair—such as osteogenic MSCs for bone regeneration and chondrogenic MSCs for cartilage repair.
However, improper differentiation poses risks, including fibrosis or unintended tissue formation, which can undermine therapeutic outcomes. Ensuring lineage specificity through controlled protocols is essential for the safety and efficacy of MSC-based therapies.
Lineage knowledge also informs scaffold design in tissue engineering. Different MSC lineages require tailored physical and biochemical environments—stiffer scaffolds support osteogenesis, while softer matrices favor adipogenesis.
In clinical applications, precise control over MSC lineage enhances both treatment effectiveness and long-term integration, making it a foundational aspect of cell therapy and regenerative design.
